If you've noticed your body odor changing during puberty, pregnancy, menopause, or other hormonal transitions, you're not imagining things. These shifts in scent aren't just about increased sweating—they're rooted in how hormones reshape the bacterial communities living on your skin.
The Microbiome-Hormone Connection
Fresh sweat is actually odorless. The distinctive smells we associate with body odor only emerge when skin bacteria metabolize compounds in our sweat. When hormones fluctuate, they alter the composition of apocrine gland secretions in areas like the armpits and intimate regions, changing what "food" is available for bacteria. This creates an environment where certain bacterial species thrive while others diminish, fundamentally shifting your body's scent profile.
The Bacterial Culprits Behind Different Odors
Different bacterial species produce distinctly different smells. Understanding which bacteria are causing your odor can be the first step toward addressing it:
Corynebacterium species are among the most significant contributors to body odor. These bacteria produce volatile fatty acids that create various unpleasant scents. Corynebacterium striatum and Corynebacterium jeikeium generate 3-methyl-2-hexenoic acid (3M2H), which produces a goat-like odor, while 3-hydroxy-3-methylhexanoic acid (HMHA) creates a distinctive cumin-like smell. Studies show that higher abundances of Corynebacterium correlate directly with stronger body odor, particularly in men.
Staphylococcus hominis is responsible for one of the most offensive odor profiles—the smell of rotten onions or raw meat. This bacterium produces 3-methyl-3-sulfanylhexan-1-ol (3M3SH), a sulfur-containing compound that creates that characteristic pungent, onion-like odor many people find particularly distressing.
Bacteria causing fecal odors represent some of the most concerning and embarrassing body odor issues, particularly in intimate areas. Para-cresol (para-hydroxytoluene) is a compound that produces distinctly fecal, stable, or barn-like odors. Additionally, indole and skatole—aromatic compounds naturally present in feces—can be produced by certain bacterial species when they metabolize the amino acid tryptophan. While these compounds are less volatile than sulfur-based odors, their presence can create persistent, unpleasant fecal notes that are especially distressing. In the anogenital region, conditions like chronic constipation or bacterial imbalances can lead to hydrogen sulfide, methanethiol, and dimethyl sulfide production, all contributing to fecal-type odors. These smells often indicate a significant microbiome imbalance that requires targeted intervention.
Additional odor-producing bacteria include Propionibacterium species that metabolize glycerol and lactic acid to create acetic and propionic acids, resulting in sour, vinegar-like odors. Staphylococcus epidermidis breaks down leucine in sweat to produce isovaleric acid, creating the characteristic cheesy smell often associated with foot odor. Anaerococcus and Peptoniphilus species, while less abundant, can also contribute to overall malodor intensity, particularly in males where these bacteria are more prevalent.
Why Hormones Matter
Hormonal changes don't just increase sweat production—they fundamentally alter its composition. Apocrine glands, which become active during puberty, secrete proteins, lipids, steroids, and hormones that serve as a feast for certain bacteria. During pregnancy, menopause, menstrual cycles, or conditions affecting hormone balance, these secretions change in ways that can favor odor-producing bacterial species over beneficial ones.
Men typically have larger apocrine glands and higher Corynebacterium populations, which explains why male body odor often has that fatty, acid-spicy, or goat-like quality. Women generally have more Staphylococcus species and may experience more sulfury, onion-like notes. These differences become more pronounced during hormonal fluctuations.
A New Approach to Odor: Precision Microbial Solutions
For years, people have masked body odor with deodorants or tried to eliminate bacteria with antiperspirants. But these approaches often backfire—antiperspirants can actually increase populations of odor-producing bacteria by creating stress conditions that favor resistant strains.
Parallel Health's innovative approach offers something different. The MD-03 Odor Protocol™ recognizes that you are unique, providing every patient with the Odor Discovery Test—a comprehensive microbiome analysis that identifies exactly which bacteria are responsible for your unique odor profile. Rather than guessing, you'll know your Odor Microbiome Type™ and understand the specific bacterial imbalances causing your scent.
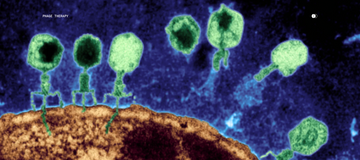
Based on these results, and if there's a bacterial match, Parallel assigns a Custom Active Phage Serum™ tailored to your microbiome. Phage therapy uses bacteriophages—nature's precision tools—that target only the specific odor-causing bacteria while leaving beneficial microbes intact. Unlike broad-spectrum antimicrobials that disrupt your entire skin ecosystem, phages work with surgical precision to rebalance your microbiome naturally.
The MD-03 Odor Protocol™ combines this cutting-edge phage therapy with ongoing clinical guidance from doctors and scientists who specialize in microbiome health, offering a long-term solution rather than temporary masking. Many users report noticeable reductions in odor within weeks, with lasting improvements as their microbiome rebalances.
Understanding that body odor stems from microbial imbalances rather than personal hygiene failures is empowering. Hormonal changes are natural, but living with distressing body odor doesn't have to be. By identifying the specific bacteria causing your odor and using targeted, natural solutions like phage therapy, you can address the root cause rather than simply covering up symptoms.
Your body's scent tells a story about the microbial ecosystem living on your skin. With the right tools to read and respond to that story, you can write a new chapter—one where hormonal changes don't have to mean accepting unwanted odors.
Frequently Asked Questions
Q: Why does my body odor change during my menstrual cycle?
A: Hormonal fluctuations throughout your cycle alter the composition of apocrine gland secretions. These changes affect which bacteria thrive on your skin, leading to different odor profiles during different phases of your cycle. Many women notice stronger or different odors during ovulation and just before menstruation when hormone levels shift most dramatically.
Q: Is it normal for body odor to suddenly change during menopause or perimenopause?
A: Absolutely. Declining estrogen levels during perimenopause and menopause significantly impact sweat gland activity and composition. These hormonal shifts can change your skin's pH and the nutrients available to bacteria, often resulting in new or intensified body odors that weren't present before.
Q: Can pregnancy cause different types of body odor?
A: Yes. Pregnancy causes dramatic hormonal changes that affect sweat production and composition. Many pregnant women notice stronger odors or entirely different scent profiles. This occurs because elevated hormone levels alter what the apocrine glands secrete, which in turn changes bacterial activity on the skin.
Q: Will my body odor return to normal after hormonal changes stabilize?
A: It depends. Sometimes the bacterial community shifts permanently to a new stable state. However, with targeted interventions like phage therapy that rebalance the microbiome, it's possible to shift toward a less odorous bacterial profile even after hormonal changes have occurred.
Q: Why do traditional deodorants sometimes make my odor worse?
A: Antiperspirants can actually increase populations of odor-producing bacteria. When you eliminate bacteria with harsh antimicrobials, the survivors tend to be stress-tolerant, potentially more odorous strains. These resistant bacteria then repopulate your skin, sometimes creating worse odor than before.
Q: How is phage therapy different from using antibacterial products?
A: Phage therapy uses bacteriophages that target only specific problem bacteria while leaving beneficial microbes intact. Unlike broad-spectrum antimicrobials that wipe out your entire microbiome, phages work with precision to rebalance bacterial populations naturally. This creates lasting improvements rather than temporary masking.
Q: How long does it take to see results from microbiome-based odor treatments?
A: Many people using Parallel Health's MD-03 Odor Protocol™ notice reduced odor within the first month. However, achieving optimal microbiome balance typically takes several months as beneficial bacteria establish themselves and odor-causing species diminish.
Q: Are certain ethnicities more prone to specific types of body odor?
A: Yes, genetics play a significant role. For instance, a variation in the ABCC11 gene, common in East Asian populations, results in reduced body odor because it limits the secretion of odor precursors. Different genetic backgrounds can also influence which bacterial species colonize the skin.
Scientific References
-
Callewaert, C., Lambert, J., & Van de Wiele, T. (2017). Towards a bacterial treatment for armpit malodour. Experimental Dermatology, 26(5), 388-391.
-
Troccaz, M., Gaia, N., Beccucci, S., Schrenzel, J., Cayeux, I., Starkenmann, C., & Lazarevic, V. (2015). Mapping axillary microbiota responsible for body odours using a culture-independent approach. Microbiome, 3, 3.
-
Fredrich, E., Barzantny, H., Brune, I., & Tauch, A. (2013). Daily battle against body odor: towards the activity of the axillary microbiota. Trends in Microbiology, 21(6), 305-312.
-
Mogilnicka, I., Bogucki, P., & Ufnal, M. (2020). Microbiota and malodor—Etiology and management. International Journal of Molecular Sciences, 21(8), 2886.
-
James, A. G., Austin, C. J., Cox, D. S., Taylor, D., & Calvert, R. (2013). Microbiological and biochemical origins of human axillary odour. FEMS Microbiology Ecology, 83(3), 527-540.