The mirror tells a story. Every fine line, every subtle fold, every change in texture—they all trace back to what's happening beneath the surface. Understanding why skin ages isn't just about tracking time or counting expressions. It's about cellular biology, structural protein degradation, and something most people never consider: the trillions of bacteria living on your skin.
When we think about anti-aging skincare, we often focus on what we can see: wrinkles forming, elasticity fading, texture roughening. But the real action happens at the molecular level, where your skin's microbiome, collagen matrix, cellular energy systems, and inflammatory responses converge to determine how your skin ages—and how it looks.
The Biology Behind Aging Skin
The eye area is where aging tends to show up first, and there's a reason for that. The periorbital skin is approximately 40% thinner than the rest of your face, with fewer oil glands and a more delicate composition. But aging doesn't stop at the eyes—it manifests differently across your entire face based on skin thickness, muscle activity, and environmental exposure.
Facial muscles contract thousands of times per day as you smile, frown, squint, and speak. The orbicularis oculi muscle around your eyes, the frontalis muscle on your forehead, and the muscles around your mouth all create repetitive dynamic movements. Over time, these contractions create creases that eventually become static lines visible even at rest—crow's feet around the eyes, horizontal lines across the forehead, and nasolabial folds around the mouth.
As we age, two critical structural proteins decline: collagen and elastin. Collagen provides firmness and structure throughout the dermis, while elastin gives skin its ability to bounce back. This natural degradation is accelerated by UV exposure, which breaks down collagen faster through the generation of matrix metalloproteinases (MMPs)—enzymes that dismantle the dermal matrix across your entire face. Add in factors like oxidative stress, chronic inflammation, and compromised skin barrier function, and you have a cascade of processes that manifest as visible aging wherever your skin is vulnerable.
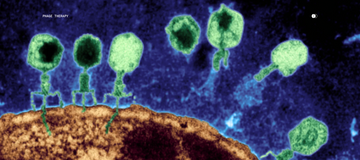
The Microbiome Connection
What's often overlooked in discussions about facial aging is the role of the skin microbiome. The billions of microorganisms living on and in your skin don't just sit there—they actively influence skin health, barrier function, and inflammatory responses across your entire face. Recent research published in the British Journal of Dermatology reveals that the skin microbiome is directly associated with visible aging appearance. Some bacterial species can accelerate skin aging, while others promote delayed aging by maintaining a more resilient microbial community. Remarkably, certain skin bacteria even help protect against UV absorption and modulate immune responses to sun exposure—factors that directly impact both cellular aging and visible skin appearance.
When the skin microbiome is disrupted, it can lead to increased inflammation and accelerated degradation of the extracellular matrix, making fine lines and wrinkles more pronounced throughout your face. A balanced skin microbiome supports barrier integrity, helps regulate immune function, and produces metabolites that can influence skin aging. This is where precision microbiome dermatology enters the picture.
Why Botox Works (But Doesn't Fix Everything)
Botulinum toxin injections have become the gold standard for treating dynamic wrinkles across the face, and for good reason—they work.
By blocking acetylcholine release at neuromuscular junctions, Botox temporarily paralyzes targeted facial muscles, preventing the repetitive contractions that create and deepen dynamic wrinkles. Whether it's the orbicularis oculi around the eyes, the frontalis on the forehead, or the corrugator muscles between the brows, the results are visible, predictable, and relatively quick.
But Botox isn't a complete solution. It doesn't rebuild lost collagen. It doesn't repair your skin barrier. It doesn't address the UV damage that's been accumulating in your dermal matrix. It doesn't modulate the inflammatory processes or support your skin microbiome. And it certainly doesn't enhance cellular energy metabolism or provide the building blocks your fibroblasts need to synthesize new structural proteins.
In other words, Botox treats a symptom—muscle contraction in specific areas—while the underlying causes of aging skin continue. Your collagen is still degrading. Matrix metalloproteinases are still breaking down your extracellular matrix. Oxidative stress is still damaging cellular structures. The moment Botox wears off (typically 3-4 months), those same aging processes are waiting, often having progressed further during that time.
This is why a comprehensive approach to facial aging needs to address multiple mechanisms simultaneously: muscle activity, collagen synthesis, barrier function, cellular energy, and microbiome health (read about how Parallel defines skin aging: 7 Hallmarks of Aging™). It's not about choosing between intervention and prevention—it's about supporting your skin's biological capacity to maintain and repair itself across your entire face.
Add Microbiome-Supportive Precision Peptide Technology
The Blue Biotic™ Multi-Effect Peptide Cream takes a multi-pronged approach to addressing wrinkles and fine lines. It harnesses peptides—short chains of amino acids that act as cellular messengers—to target both the visible symptoms and underlying causes of periorbital aging.
The formulation contains SNAP-8 (Acetyl Glutamyl Heptapeptide-1), a neuropeptide that functions as a topical muscle relaxant. SNAP-8 works by blocking neuromuscular signals that trigger muscle contractions, similar to the mechanism of Waglerin-1-mimicking compounds. By temporarily reducing repetitive muscle movements, this peptide helps prevent the deepening of dynamic wrinkles without injections or toxins.
But the innovation doesn't stop there. The Blue Biotic™ also incorporates Matrixyl 3000™ and copper peptides, a powerful combination that addresses volume loss and stimulates collagen production. Matrixyl 3000 contains palmitoyl oligopeptides that activate fibroblasts—the cells responsible for producing new collagen and elastin—by mimicking signals found in thrombospondin-1, a protein involved in tissue regeneration. Copper peptides enhance this effect by promoting collagen synthesis, supporting wound healing, and reducing inflammatory signals that accelerate matrix degradation.
The formulation is rounded out with beta-glucan, which supports skin healing and barrier repair, and topical creatine, which enhances cellular energy metabolism—helping skin cells function more efficiently as they work to maintain and repair tissue. This multi-mechanism approach doesn't just address surface-level concerns—it targets the biological processes that drive visible aging at the cellular level.
Moving Beyond Beauty to Skin Longevity
Maintaining youthful-looking eyes isn't just about vanity. The eye area is a visible reflection of cellular health, barrier function, and the complex interplay between your skin and its resident microbiome. When you support skin health at the microbial and cellular level—whether through microbiome-compatible products like the Blue Biotic™ or by protecting against environmental stressors—you're investing in the long-term resilience and vitality of your skin.
Because healthy skin isn't just about looking younger. It's about supporting the biological systems that keep your skin functioning optimally, for years to come.
Frequently Asked Questions
Q: At what age do crow's feet typically start to appear?
Most people begin noticing crow's feet in their late twenties to early thirties, though this varies based on genetics, skin microbiome, sun exposure, and lifestyle factors. The periorbital area shows aging signs earlier because the skin is thinner and has fewer oil glands than other facial areas.
Q: Can peptides really work like Botox without injections?
Peptides like SNAP-8 work through a different mechanism than Botox but achieve similar results by temporarily reducing muscle contractions that cause dynamic wrinkles. While they're not as potent as neurotoxin injections, topical peptides offer a non-invasive alternative with cumulative benefits when used consistently.
Q: How long does it take to see results from the Blue Biotic™?
You may notice improved hydration and texture within 1-2 weeks, but visible reduction in fine lines typically requires 8-12 weeks of consistent use as the multiple peptides work in synergy to stimulate collagen production and modulate muscle activity over time.
Q: How does the skin microbiome affect facial aging?
According to research published in the British Journal of Dermatology, the composition of your skin microbiome directly influences visible aging. Certain bacterial species can accelerate skin aging through inflammatory pathways, while others promote a more resilient skin barrier and even offer protection against UV damage—all factors that impact how your face ages.
Q: Is it safe to use peptide creams on my entire face?
Yes, peptides are generally well-tolerated and safe for use across the face, including delicate areas like around the eyes. However, if you have sensitive skin or specific concerns, it's always advisable to patch test new products and consult with a dermatologist.
Q: Can I use the Blue Biotic™ with other anti-aging products?
The Blue Biotic™ is designed to complement a comprehensive skincare routine. It can be layered with other serums and moisturizers, though it's best to apply it after cleansing. The Blue Biotic™ can also be used with Parallel's Custom Anti-Aging Rx (see the Anti-Aging Duo), which contains prescription-grade levels of tretinoin and other ingredients specific to your skin. Always use sunscreen during the day, as sun protection is crucial for preventing further periorbital aging.
References
-
Xu YN, Pu M, Raut J, et al. Skin microbiome as a signature of premature ageing appearance: Manipulation through by use of topical products. Br J Dermatol. 2025. DOI: 10.1093/bjd/ljaf098
-
Harel N, Ogen-Shtern N, Reshef L, et al. Skin microbiome bacteria enriched following long sun exposure can reduce oxidative damage. Res Microbiol. 2023;174(8):104138. DOI: 10.1016/j.resmic.2023.104138
-
Lee JS, Min JW, Gye SB, et al. Suppression of UVB-Induced MMP-1 Expression in Human Skin Fibroblasts Using Lysate of Lactobacillus Derived from Korean Women's Skin in Their Twenties. Curr Issues Mol Biol. 2024;46(1):513-526. DOI: 10.3390/cimb46010033
-
Liu MM, Tian ZY, Wang YM, Wang QM. Enhancement of skin defense against UVB damage by fermentation of Leonurus japonicus with Saccharomyces cerevisiae. Phytomedicine. 2025;147:157206. DOI: 10.1016/j.phymed.2025.157206
-
Shen C, Zhou X, Jiang J, et al. Injectable amino-modified poly-L-lactic acid microspheres/hyaluronic acid-based hydrogel composites for soft tissue fillers. Biomater Adv. 2025;178:214465. DOI: 10.1016/j.bioadv.2025.214465
-
Zhou Z, Bu Z, Wang S, et al. Extracellular matrix hydrogels with fibroblast growth factor 2 containing exosomes for reconstructing skin microstructures. J Nanobiotechnology. 2024;22(1):438. DOI: 10.1186/s12951-024-02718-8
-
Zhang Q, Kong L, Wang Q, et al. A biotin-stabilized HKUST-1/ADM scaffold for facilitating MSC endothelial differentiation and vascularization in diabetic wound healing. Biomater Sci. 2023;11(3):854-872. DOI: 10.1039/d2bm01443b
-
Cao Y, Wang P, Zhang G, et al. Administration of skin care regimens containing β-glucan for skin recovery after fractional laser therapy: A split-face, double-blinded, vehicle-controlled study. J Cosmet Dermatol. 2020;20(6):1756-1762. DOI: 10.1111/jocd.13798
-
Petrović J, Glamočlija J, Milinčić DD, et al. Comparative Chemical Analysis and Bioactive Properties of Aqueous and Glucan-Rich Extracts of Three Widely Appreciated Mushrooms. Pharmaceuticals (Basel). 2024;17(9):1153. DOI: 10.3390/ph17091153
-
Zemtsov A, Montalvo-Lugo V. Topically applied growth factors change skin cytoplasmic creatine kinase activity and distribution and produce abnormal keratinocyte differentiation in murine skin. Skin Res Technol. 2008;14(3):370-375. DOI: 10.1111/j.1600-0846.2008.00287.x