By 2050, Over 40 Million People Will Die from an Antibiotic Resistance Infection: The Rising Threat of Antimicrobial Resistance
by Parallel Health Team
We have long heard about the overuse of antibiotics and the future dangers of antibiotics. However, a recent study published in The Lancet makes it known that we must face these dangers now. The recent study projects a staggering 40 million deaths linked to antimicrobial resistance (AMR) over the next 25 years, further indicating the burden of the ongoing superbug crisis.
Researchers compiled data from over 520 million records across 204 countries, analyzing 22 pathogens, 84 pathogen-drug combinations, and 11 infectious syndromes, including meningitis and bloodstream infections. The implications of this study underscore the urgent need to address AMR before it spirals further out of control, affecting not only individual health but also our healthcare systems globally.
What is Antimicrobial Resistance? Antimicrobial resistance occurs when bacteria, viruses, fungi, and parasites change in response to the medications used to treat them. When bacteria become resistant, the drugs that used to work no longer do, making it harder to cure infections and increasing the risk of severe illness or death.
The Role of Overuse and Misuse of Antibiotics in AMR: One of the primary drivers of AMR is the overprescription and misuse of antibiotics. As patients, you may have experienced a time when you requested antibiotics for a cold or the flu, thinking they would help you recover faster. However, it’s crucial to understand that antibiotics are ineffective against viral infections. When healthcare providers prescribe antibiotics unnecessarily or chronically, it can lead to significant problems.
Additionally, many people stop taking their antibiotics once they start feeling better, believing they no longer need the medication. This premature discontinuation can allow the most resilient bacteria to survive and multiply, leading to antibiotic resistance. Over time, these resistant strains can make previously treatable infections more difficult, if not impossible, to manage.
The seriousness of AMR cannot be overstated. Bacterial infections that were once easily treatable are becoming increasingly difficult to manage due to resistance. This phenomenon not only leads to higher morbidity and mortality rates but also places a substantial burden on healthcare systems. Patients with resistant infections often require longer hospital stays, more intensive care, and the use of more expensive and potentially toxic alternatives.
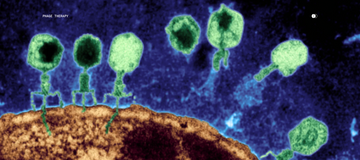
Our Commitment to Combating AMR: As a company focused on innovative health solutions, Parallel is dedicated to developing phage cosmeceuticals and therapies as effective and safe alternatives to traditional antibiotics.
Bacteriophages, or phages, are nano-microbes that specifically target and kill bacteria without harming human cells or beneficial microbes. This targeted action allows phages to eliminate harmful bacteria while preserving the microbiome, reducing the risk of disruption. Unlike antibiotics, phages can also adapt to evolving bacteria, making them a sustainable solution against resistant infections. Additionally, phages typically have fewer side effects than antibiotics, leading to better patient experiences. Importantly, the unique killing mechanism of phages reduces the likelihood of bacteria developing resistance, providing a promising alternative in the fight against AMR.
At Parallel, we understand that AMR is more than just a medical issue; it’s a global health crisis that needs our immediate attention. We’re committed to developing bacteriophage therapies as effective, safe alternatives to antibiotics, starting with dermatology, where antibiotics are prescribed the most out of any healthcare specialty. Together, we can fight AMR and safeguard our health for the future.