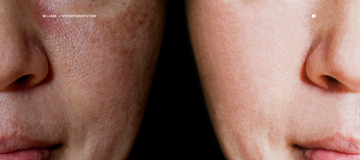
If you've noticed dark, patchy discoloration on your face that seems resistant to your usual skincare routine, you're not alone. Melasma affects millions of people worldwide, and while it's medically benign, its impact on confidence and quality of life is very real. Understanding this complex condition is the first step toward finding an effective treatment approach.
What Is Melasma?
Melasma is a chronic pigmentation disorder characterized by brown or gray-brown patches, typically appearing symmetrically on the face—particularly the cheeks, forehead, upper lip, and chin. Unlike other forms of hyperpigmentation, melasma is notoriously stubborn and multifactorial, making it challenging to treat with conventional approaches alone.
Distinguishing Melasma from Other Pigmentation Issues:
While all involve excess melanin production, these conditions differ in their causes and patterns. Sunspots (solar lentigines) are isolated, well-defined spots caused by cumulative UV damage, typically appearing on sun-exposed areas in older adults. General hyperpigmentation is an umbrella term for any darkened skin area, often resulting from inflammation, injury, or acne. Melasma, however, presents as larger, symmetric patches triggered by hormonal factors, appearing most commonly on the face with a characteristic pattern. Its hormonal-inflammatory-microbial nature makes it uniquely complex and persistent compared to sun damage or post-inflammatory darkening.
The Hormonal Connection
One of melasma's most well-established triggers is hormonal fluctuation. Studies show that up to 50-70% of pregnant women develop melasma, often called the "mask of pregnancy." Similarly, oral contraceptives and hormone replacement therapy are strongly associated with melasma development. This hormonal link explains why melasma disproportionately affects women, though men can develop it too.
The mechanism involves estrogen and progesterone stimulating melanocytes—the pigment-producing cells in our skin—making them hyperresponsive to other triggers like UV exposure. This is why melasma often appears or worsens during pregnancy, while taking birth control, or during hormonal transitions.
The Emerging Microbiome Connection
Recent research has revealed a fascinating new dimension to melasma: the skin microbiome. Published studies have found that individuals with melasma show distinct differences in their skin bacterial composition compared to those without the condition. Specifically, overgrowth of certain bacterial species, particularly Cutibacterium acnes (formerly Propionibacterium acnes), has been associated with melasma lesions.
This discovery suggests that dysbiosis—an imbalance in the skin's microbial ecosystem—may contribute to the inflammatory processes that trigger excess pigmentation. Certain bacteria can produce metabolites that activate melanocytes or create low-grade inflammation, perpetuating the pigmentation cycle.
Beyond UV Exposure
While sun protection remains crucial in managing melasma, UV exposure is just one piece of the puzzle. Heat, visible light, and even blue light from screens can all trigger melanocyte activity. This explains why melasma can persist or worsen despite diligent sunscreen use.
A Personalized Approach to Treatment
Given melasma's complex, multifactorial nature, a personalized treatment strategy is essential. At Parallel Health, we recognize that effective melasma management requires understanding your unique triggers—including your skin microbiome composition.
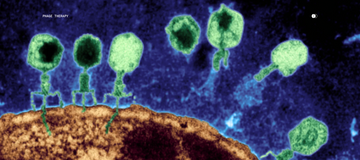
Our comprehensive approach looks to understand your clinical history and hormonal triggers, but also includes skin microbiome testing to identify potential bacterial imbalances contributing to your melasma. Based on these insights, we can develop targeted interventions, including innovative phage therapy to selectively modulate problematic bacterial populations without disrupting your beneficial skin flora. Combined with custom-compounded prescription formulations tailored to your specific needs, this integrative approach addresses melasma from multiple angles.
Understanding that melasma is more than skin-deep—encompassing hormonal, environmental, and microbial factors—empowers you to pursue more effective, personalized solutions for clearer, more even-toned skin.
Scientific References
-
Handel AC, et al. Risk factors for facial melasma in women: a case-control study. British Journal of Dermatology. 2014;171(3):588-594.
-
Kwon SH, et al. Heterogeneous pathology of melasma and its clinical implications. International Journal of Molecular Sciences. 2016;17(6):824.
-
Skowron K, et al. Human skin microbiome: Impact of intrinsic and extrinsic factors on skin microbiota. Microorganisms. 2021;9(3):543.
-
Jang YH, et al. Differences in microbial community structure between melasma skin and adjacent unaffected skin. Journal of Dermatological Science. 2020;99(1):12-19.
-
Kang HY, Ortonne JP. What should be considered in treatment of melasma. Annals of Dermatology. 2010;22(4):373-378.
Frequently Asked Questions
Q: Will my melasma go away after pregnancy or stopping birth control?
A: While hormonal melasma may fade after pregnancy or discontinuing hormonal contraceptives, it often persists without treatment. The pigmentation can become chronic, especially with continued sun exposure.
Q: How is the skin microbiome related to melasma?
A: Research shows that melasma-affected skin has different bacterial populations compared to healthy skin. Certain bacteria may produce inflammatory compounds or metabolites that trigger excess melanin production, contributing to persistent pigmentation.
Q: What is phage therapy for melasma?
A: Phage therapy uses bacteriophages—nano-microbes that specifically target bacteria—to selectively reduce problematic bacterial populations on the skin without harming beneficial microbes. This precision approach can help restore skin microbiome balance.
Q: Can melasma be cured?
A: Melasma is considered a chronic condition that requires ongoing management rather than a one-time cure. However, with comprehensive treatment addressing hormonal, environmental, and microbial factors, significant improvement and long-term control are achievable.
Q: How long does it take to see results from microbiome-based treatments?
A: Skin cell turnover takes approximately 28 days, so initial improvements typically appear within 4-8 weeks. However, optimal results often require 3-6 months of consistent treatment as the skin microbiome rebalances and pigmentation gradually fades.