Semaglutide and other GLP-1s deliver dramatic results—but new research reveals they're reshaping your gut microbiome in unexpected ways. The downstream effects on your skin and oral microbiomes, immunity, and long-term health are only now coming into focus.
The Unexamined Trade-Off
GLP-1 receptor agonists like Ozempic, Wegovy, and Mounjaro have become the most talked-about medications in a generation. The results speak for themselves: 5–18% body weight reductions in clinical trials, improved metabolic markers, and cardiovascular benefits.
However, these drugs fundamentally alter your gut environment for better or worse. A 2025 systematic review analyzing 38 studies found that the effects vary significantly depending on which GLP-1 you're taking and the state of your microbiome beforehand.
Not All GLP-1s Are Created Equal
The research reveals important differences between medications. In studies comparing microbiomes before and after treatment, several GLP-1s actively shifted bacterial populations, but the direction of that shift varies.
Liraglutide and dulaglutide both consistently promoted growth of beneficial genera including Lactobacillus, Akkermansia muciniphila, Bacteroides, and Ruminococcus—species associated with improved metabolic health, stronger gut barriers, and reduced inflammation.
Semaglutide also boosted Akkermansia muciniphila and other beneficial species, but it also reduced overall microbial diversity in multiple studies. Diversity loss is typically a red flag in microbiome science, associated with inflammation and immune dysregulation. While short-term metabolic benefits are clear, the long-term implications of reduced diversity remain unknown.
There is so much more we need to (and will be learning) about how GLP-1s affect our long-term health. But one thing is clear: they actively reshape your microbial ecosystem–sometimes favorably, sometimes with trade-offs that warrant monitoring. Your specific response likely depends on which medication you're taking, your baseline microbiome, and how your diet changes during treatment.
The Added Problem of Starvation
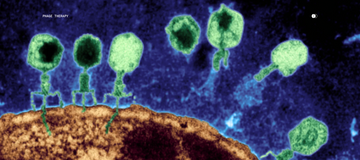
GLP-1 medications suppress appetite so effectively that users reduce caloric intake by 16–39%. That's the point, of course. But your gut bacteria didn't get the memo.
The trillions of microbes in your digestive tract depend on dietary fiber for fuel. When they ferment fiber, they produce short-chain fatty acids—compounds essential for gut barrier integrity, immune regulation, and controlling inflammation throughout your body, including your skin.
Fewer than 5% of Americans meet fiber recommendations before starting these medications. When food intake drops by a third, fiber intake often collapses. You may be inadvertently starving the very bacteria that keep you healthy—creating a state of dysbiosis that persists even as the scale moves in the right direction.
Your Skin May Be Paying the Price
The gut-skin axis is well-established science. Gut dysbiosis triggers systemic inflammation and immune responses that manifest on the skin as acne, rosacea, eczema, and accelerated aging. A 2022 review in Gut Microbes documented the mechanisms clearly.
While no published studies have yet directly measured skin microbiome changes in GLP-1 users, the biological connections are compelling. As millions of people are now taking these medications, more research is needed to understand how these drugs affect not just the gut, but the interconnected microbial ecosystems across your body.
This is where precision testing becomes valuable. With Parallel Health's microbiome technology, we can begin to explore how GLP-1s are affecting your skin, scalp, oral and gut microbiomes at the individual level—giving you real data rather than waiting years for population-level studies to catch up.
What You Can Do Now
The goal isn't to alarm you off effective medication—it's to ensure you're not trading one problem for another.
Prioritize fiber aggressively. Even with reduced appetite, target 25–35g daily through vegetables, legumes, and whole grains. Your microbiome depends on it.
Monitor your body. New skin issues, persistent digestive symptoms, changes in hair or oral health—these may signal microbiome disruption worth investigating.
Consider precision testing. Generic supplements won't cut it. Understanding your specific microbiome state allows for targeted interventions based on what's actually happening in your body, not population averages that may not apply to you.
GLP-1 medications are powerful tools. But powerful tools require precision—not just in dosing, but in supporting the ecosystem that determines how your body responds.
Frequently Asked Questions
Do GLP-1 medications directly harm the microbiome?
The evidence doesn't support a simple "harmful" label. Studies show mixed effects: some beneficial bacteria increase while overall diversity may decrease (particularly with semaglutide). The effects appear to vary significantly between individuals and depend heavily on diet during treatment. Many changes may be indirect—resulting from reduced food intake and altered gut motility rather than direct drug effects on bacteria.
Can microbiome changes from GLP-1 medications affect my skin?
We know GLP-1 medications change gut microbiota. In line with the confirmation of the gut-skin axis, we know that gut microbiome changes can trigger skin inflammation, alter immune responses, and affect skin barrier function. However, clinical studies specifically measuring skin microbiome changes in GLP-1 users haven't yet been published.
Should I take probiotics while on GLP-1 medications?
The effectiveness of probiotics depends on your specific microbiome state, which strains you need, and whether they can survive to colonize your gut. Precision testing can identify whether you're deficient in specific beneficial bacteria and guide targeted interventions rather than random supplementation.
How soon might I notice microbiome-related changes after starting GLP-1 therapy?
Gut microbiome shifts can begin within days to weeks of significant dietary changes. Skin manifestations of gut changes may take longer—weeks to months—as they depend on systemic inflammation and immune signaling cascades. If you notice new skin issues, digestive changes, or oral health changes within the first few months of GLP-1 therapy, microbiome involvement is worth considering.
What's the difference between gut microbiome testing and skin microbiome testing?
These are distinct ecosystems with different compositions and functions. Gut microbiome testing (typically via stool samples) reveals your intestinal bacterial populations and their metabolic functions. Skin microbiome testing identifies the bacteria colonizing your skin surface, which can influence acne, aging, barrier function, and inflammation. For comprehensive insight, both may be valuable, particularly if you're experiencing both digestive and skin changes.
Are some GLP-1 medications better or worse for the microbiome?
Early evidence suggests different GLP-1 medications may have different microbiome profiles. The 2025 systematic review noted that liraglutide promoted growth of beneficial genera, while semaglutide showed more variable effects with potential diversity reductions. However, these differences need more research and likely depend heavily on individual factors. Your response to a specific medication may differ from population averages.
Can I prevent microbiome disruption while taking GLP-1 medications?
Optimizing dietary quality is your primary lever. Prioritizing fiber-rich foods (vegetables, legumes, whole grains), adequate protein, and nutrient density, even with reduced overall intake, supports beneficial bacteria. Staying hydrated, managing GI side effects proactively, and monitoring for changes also helps. Baseline microbiome testing before or early in treatment provides a reference point for tracking changes.
Is "Ozempic face" related to microbiome changes?
The volume and collagen loss associated with rapid weight loss ("Ozempic face") is primarily attributed to fat loss in facial compartments, not directly to microbiome changes. However, microbiome health does influence skin quality, collagen metabolism, and inflammation—all factors in skin aging. While not the primary driver, optimizing microbiome health and using collagen-producing peptides during weight loss support skin quality, volume, and resilience.
References
- Gofron KK, et al. Effects of GLP-1 Analogues and Agonists on the Gut Microbiota: A Systematic Review. Nutrients. 2025;17(8):1303.
- Ma Q, et al. Crosstalk between glucagon-like peptide 1 and gut microbiota in metabolic diseases. mBio. 2024;15(1):e02032-23.
- Mahmud MR, et al. Impact of gut microbiome on skin health: gut-skin axis observed through the lenses of therapeutics and skin diseases. Gut Microbes. 2022;14(1):2096995.
- Mozaffarian D, et al. Nutritional Priorities to Support GLP-1 Therapy for Obesity. The American Journal of Clinical Nutrition. 2025;122:344-367.
- Chen L, et al. Effects of semaglutide on metabolism and gut microbiota in high-fat diet-induced obese mice. Frontiers in Pharmacology. 2025;16:1562896.