We've been diving deep into something that's fundamentally changed how we think about skin conditions. After years of research and working with thousands of patients, we're seeing patterns that don't always match what appears on the surface.
Here's what we mean: two people can walk into a dermatologist's office with what looks like identical acne. Same severity, same location, same apparent triggers. But when we analyze their skin microbiomes at the molecular level, we often find completely different bacterial communities driving their conditions.
It's not that dermatologists are missing anything they should be seeing. Clinical observation has been the gold standard for good reason—it works for many patients. But we're learning that some answers exist at a scale that's simply invisible to the human eye.
The Microscopic Story
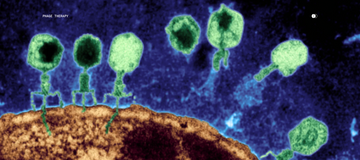
Through whole-metagenome sequencing, we can identify specific bacterial strains and their functions in ways that traditional testing can't. We're not just seeing which bacteria are present, but understanding what they're actually doing and how they're interacting with each other.
What we've discovered is that many inflammatory skin conditions aren't caused by a single "bad" bacteria. Instead, they result from complex imbalances where multiple microbial species contribute to inflammation in different ways. It's less like identifying a single culprit and more like understanding an entire ecosystem that's out of balance.
This research, which we recently published in The Dermatologist, has practical implications. It helps explain why the same treatment can work brilliantly for one person and fail completely for another, even when their conditions appear identical.
Beyond Skin
The more we learn about the skin microbiome, the more we realize how connected it is to overall health. The skin isn't just a barrier—it's an active participant in our body's ecosystem. When that ecosystem is disrupted, it can affect everything from inflammation to immune function.
That's why we're particularly interested in bacteriophage therapy. These naturally occurring microbes target specific bacterial strains with remarkable precision, leaving beneficial bacteria untouched. It's a fundamentally different approach from broad-spectrum antibiotics, which can disrupt the entire microbial community.
The Big Picture
We've created a short documentary, "Bacteriophages Could Save 40 Million Lives by 2050" that explores these ideas and their broader implications for healthcare. It examines how precision medicine approaches like bacteriophage therapy could address the growing challenge of antimicrobial resistance while providing more personalized care.
The film isn't just about our work—it's about a shift that's happening across medicine toward understanding the root causes of disease rather than just treating symptoms. We think this perspective could be transformative, not just for dermatology, but for healthcare generally.
What This Means for You
Whether you're dealing with persistent skin issues, curious about the science, or simply interested in where healthcare is heading, we believe these discoveries matter. They represent a move toward more personalized, precise treatments that work with your body's natural systems rather than against them.
We're still learning, and we're grateful to be part of this evolving understanding of human health. The microscopic world is vast and complex, but every insight brings us closer to treatments that truly address the root causes of disease.
The future of medicine might live in nano-microbes—and be more precise than we ever imagined.
To access precision care for you, sign up for the MD-03 Protocol™. Testing and precision therapies are available for face, body, scalp, and odor. Custom kits are available upon request.
Cheers to the Future of Your Skin,
Dr. Nathan Brown + Natalise Kalea Robinson